Understanding and Avoiding Migraine Triggers: Tips From a Nurse Who Gets It
Dealing with migraine attacks is tough. The first crucial step to prevent migraines is to know what triggers them. In this post, I’ll share the most common triggers and how to avoid them.
HEALTH & WELLNESS MADE SIMPLE
Sheri Anne Maximille Cabañes-Madayag
5/25/20258 min read


Note: This post is for informational purposes only and is not a substitute for professional medical advice. Please speak with your healthcare provider about your specific health concerns.
Have you ever felt your head hurt so much that you feel like chopping it off?
Throbbing pain.
Wanting to throw up.
Hating bright lights, loud noises, or strong scents.
Those were the worst days for me, having a migraine attack. I've had migraines since I was in college. I was absent from school and work for days. I also missed get-togethers with family and friends. All those were because of the unwelcome headaches.
It took me years of identifying my triggers, figuring out how to prevent migraine attacks, and consulting doctors for medical advice. I've learned that understanding what triggers migraines is the first step towards managing them.
So in this post, I will discuss migraine, common triggers, and how to prevent them.
What are migraines?
We often use the word migraine for a bad headache. While a headache always occurs in a migraine, it's more than just a headache. Migraine is a brain and nervous system disorder that includes severe headaches. Other migraine symptoms include nausea and sensitivity to light, loud noises, or strong odors.
Types of Migraine
Migraine has two main types: migraine with aura and migraine without aura.
Migraine with aura includes sensory disturbances, often visual, that occur before or during the migraine attack. The most common aura involves changes in vision, such as lights that look like stars or dots, blind spots, or temporary vision loss. Other symptoms of an aura include ringing in the ear, strange odors, or tingling sensations in a limb or on one side of the face.
Migraine without aura often involves pain on one side of the head, without the sensory disturbances, or aura, that occurs before or during the migraine attack.
Phases of Migraine
Migraine attacks occur in 4 phases: prodrome, aura, headache, and postdrome.
The prodrome phase happens up to 24 hours before the headache. Symptoms can include food cravings, unexplained mood changes, difficulty concentrating, trouble sleeping, or needing to pee more than usual.
The aura phase occurs about five minutes to an hour before or during a headache. Classic aura symptoms include vision changes and tingling in the hands or face.
A migraine headache lasts between four to seventy-two (4-72) hours. A headache is usually felt on one side of the head and often involves nausea, vomiting, sensitivity to light, smell, and sound, confusion, blurred vision, mood changes, and fatigue. It is also possible for some people to experience “silent migraines”, where they have aura or other symptoms like nausea, but no headache at all.
The postdrome phase, also known as the migraine hangover, usually lasts for a few hours up to 48 hours. Symptoms can include exhaustion, confusion, dizziness, or mood changes after a migraine.
Causes of Migraines
While the cause of migraines is unknown, migraines are believed to be influenced by genetic, environmental, and neurological factors. Research suggests that migraines are linked to changes in the nerves, chemicals, and blood flow in the brain. Genetics also plays a role. This means that a person is more likely to have migraines if someone in their family has migraines. (My mom and my aunt both have migraines, which could be why I got them.) Several factors can trigger migraines, including hormone changes, environment, stress, and food.
Understanding Migraine Triggers: The First Step to Prevention
Knowing what triggers your migraines is crucial to prevention. From my experience, I found that my triggers include a lack of sleep, several hours of hunger, foods like corn chips, and my monthly menstrual period. Below is a list of the most common migraine triggers.
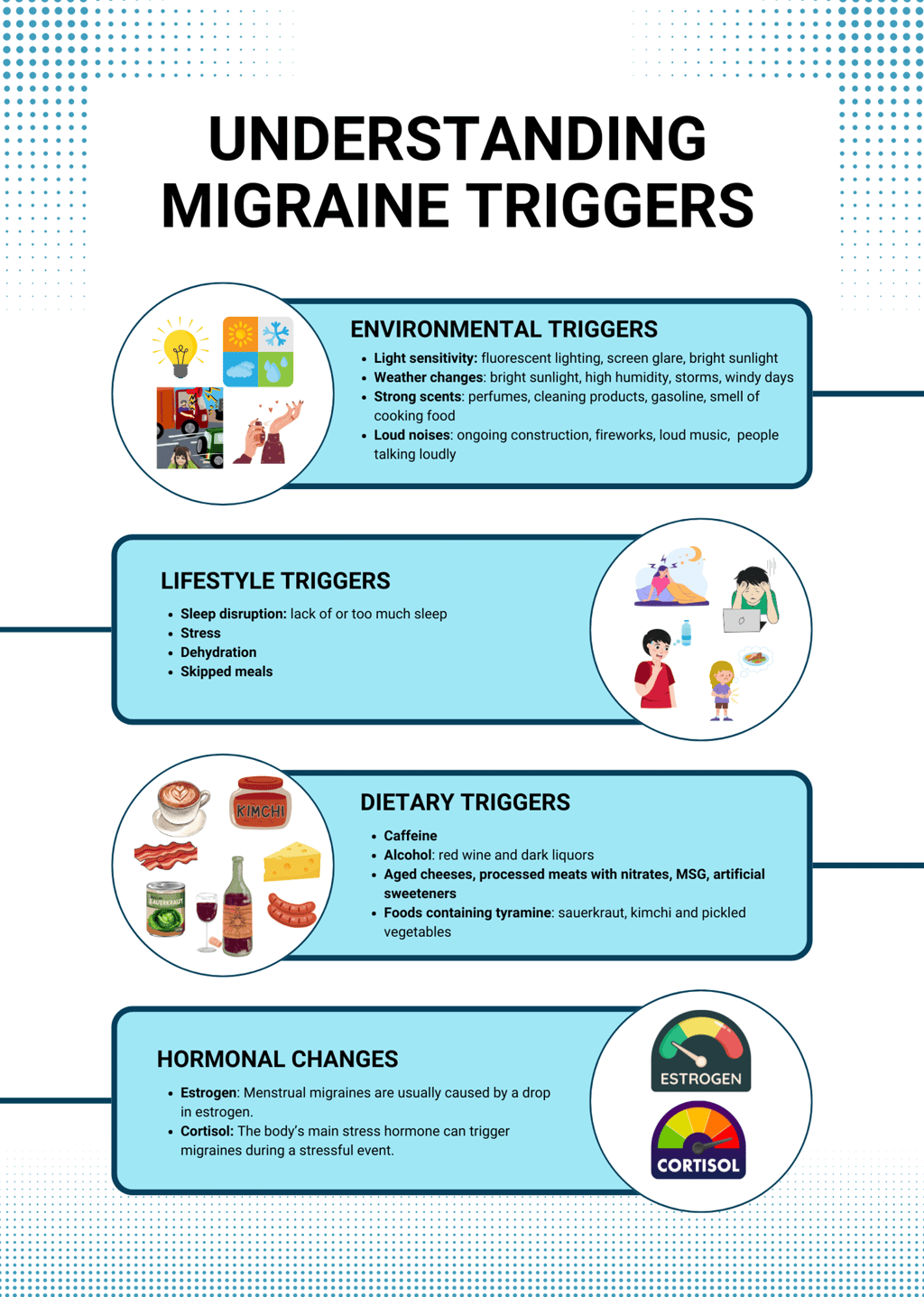
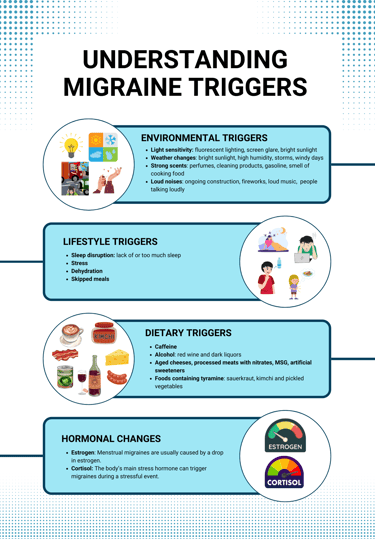
Environmental Triggers
Light sensitivity (photophobia or photosensitivity): Fluorescent lighting, screen glare, and bright sunlight can all trigger migraines. Wear sunglasses or caps when going out. Limit screen time. Adjust the lighting in your room and in your desk.
Weather changes: Extreme temperatures (heat or cold) can trigger migraines for some individuals. Bright sunlight, high humidity, storms, and windy days are the common triggers. If the weather triggers your migraine, take extra care of yourself during those times. Stay indoors. Use fans. Wear light and breathable clothes. Drink more water. Eat cold and refreshing snacks if extreme heat causes you migraines. If the cold season triggers your migraines, keep yourself warm and comfortable. Wear jackets. Use heaters or warming blankets. Drink warm drinks. Have hot meals.
Strong scents: Perfumes, cleaning products, gasoline, and certain foods cooking can also initiate an attack. Move away as quickly as possible from those smells, or wear a face mask.
Loud noises: Certain sounds, like ongoing construction, fireworks, loud music, or even people talking loudly, can trigger migraine headaches. Use earplugs or headphones, or move to a quiet place, the moment you start to hear those noises.
Lifestyle Triggers
Sleep disruption: Lack of and too much sleep can trigger migraines. Working irregular hours, like shifting schedule or the night shift, can cause sleep disruptions, increasing the risk of getting migraines. Maintain a consistent sleep schedule and practice healthy sleep hygiene to get good quality sleep. You can check out my blog post on getting quality sleep for night shift workers for more tips.
Stress: The most established universal trigger of migraines. Stress hormones, like cortisol, can cause changes in the brain's excitability and sensitivity to pain, leading to migraines. Practice stress management techniques like deep breathing and meditation. Take regular breaks at work and make sure to rest and relax on days off.
Dehydration: Lack of fluid intake is often overlooked, but can also trigger migraines by causing the brain tissues to shrink and put pressure on the nerves, which can cause headaches. Dehydration also increases sensitivity to pain, which makes migraines feel more intense. Drink at least 8 to 12 glasses of water daily. Carry a water bottle with you when going out of the house.
Skipped meals: Skipping meals or irregular meal patterns can cause hypoglycemia or low blood sugar levels, a common trigger for headaches. This is the reason why intermittent fasting never worked for me when I was trying to lose weight. Eat a healthy, balanced meal and maintain regular eating schedules.
Dietary Triggers
Caffeine: Both consumption and withdrawal can trigger migraines. I've found my sweet spot is one cup of coffee in the morning—no more, no less. Research shows that caffeine can block the effects of a chemical in the body called adenosine, which causes blood vessels to expand. It is found that adenosine levels in the blood increase during migraine attacks. In my case, not drinking coffee gives me headaches, so I have a cup just before I start work. One to two servings of caffeine (150-200 milligrams) a day might help prevent headaches. But three servings or more could increase the number of migraine attacks in a month.
Alcohol: Red wine and dark liquors are particularly known migraine triggers. It is best to avoid alcohol if it triggers your migraines. Whether or not alcohol triggers your migraine, always drink in moderation and responsibly.
Certain foods: Aged cheeses, processed meats with nitrates, MSG, artificial sweeteners, and foods containing tyramine, such as sauerkraut, kimchi and pickled vegetables, can all be triggers. Listing down the food you ate before a migraine attack can help identify if certain foods trigger your migraines. Corn chips are my nemesis, so I avoid them at all costs.
Hormonal Changes
Estrogen: Menstrual migraines are usually caused by a drop in estrogen. Studies show that at least 60% of women experience migraines around the time of their menstrual cycle. I guess I am included in that 60% because I have migraines during the first two days of my monthly period. I take extra care of myself during those times: eating healthy, hydrating properly, and getting enough rest and sleep.
Cortisol: The body’s main stress hormone can trigger migraines during a stressful event, as mentioned previously. Stress management can help regulate cortisol levels and prevent migraine attacks.
Practical Tips to Prevent Migraines

After years of being a nurse and my personal experiences with migraines, here are the migraine prevention strategies I've found most effective:
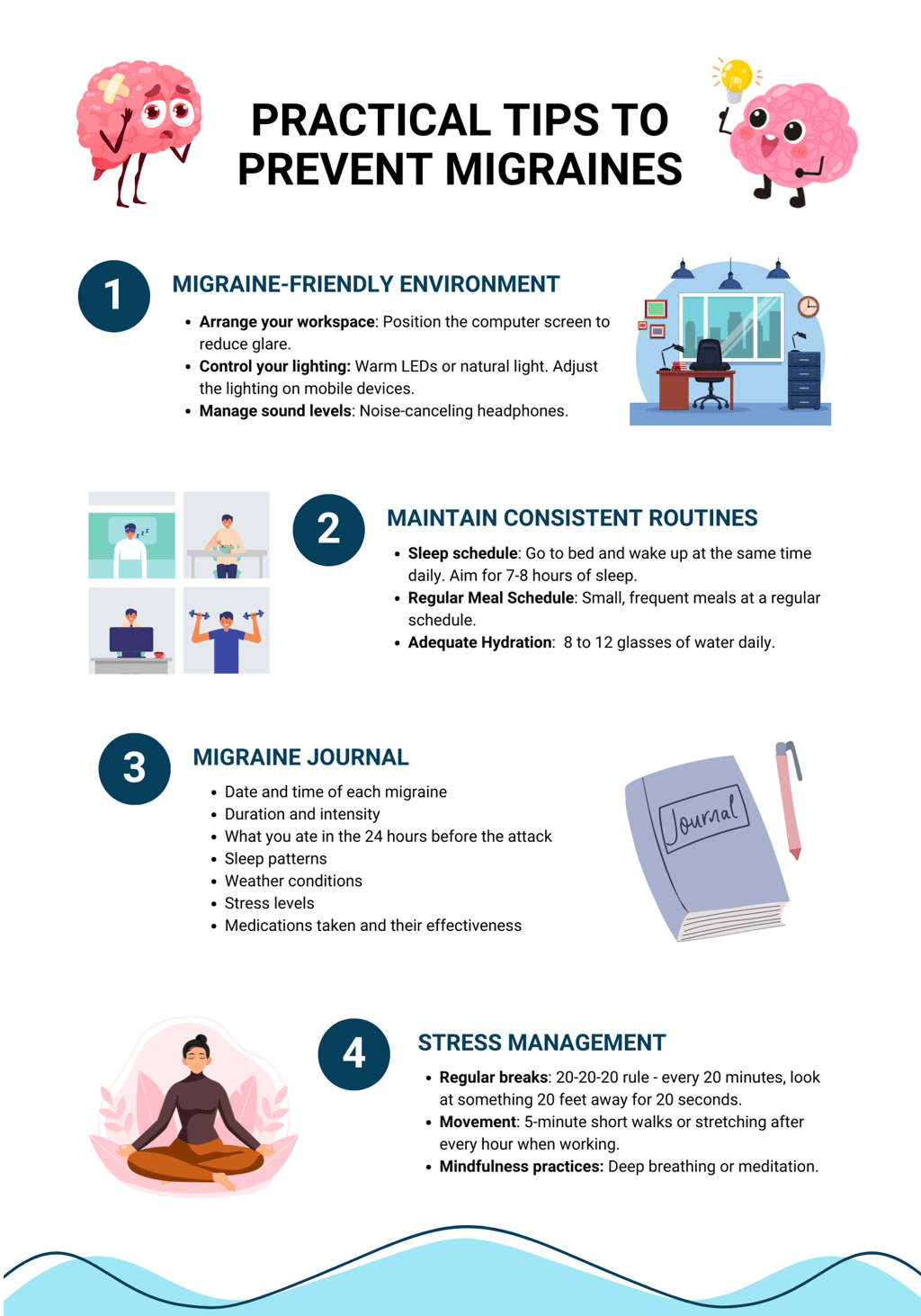
1. Create a Migraine-Friendly Environment
Arrange your workspace: Position your computer screen to reduce glare. Use anti-glare screens. Consider blue-light blocking glasses. I use blue-light blocking glasses when working on my computer. I also arranged my home office so the light comes from the side, not in front or behind me.
Control your lighting: Replace harsh fluorescent bulbs with warm LEDs or natural light options. Adjust the lighting on your mobile devices. Wear sunglasses when going out in bright sunlight or to places with bright lighting.
Manage sound levels: Use noise-canceling headphones in loud environments. Try using white noise if silence causes you headaches. I play mellow music when writing to mask distracting sounds. It also keeps me awake and focused.
2. Develop and Maintain Consistent Routines
Sleep schedule: Go to bed and wake up at the same time daily. I work night shift, but I aim to sleep for 7-8 hours.
Regular Meal Schedule: Eat small, frequent meals at a regular schedule. Avoid long gaps between heavy meals. Have a snack in between meals. I always keep healthy snacks, like a piece of fruit, bread, or some nuts, at my desk so I can have them when I'm hungry.
Adequate Hydration: Aim to drink 8 to 12 glasses of water daily. Track your water intake. Set reminders to drink. I set an hourly reminder to drink water when I'm working so I always stay hydrated.
3. Keep a Migraine Journal
Keeping track of your migraine attacks through a migraine journal or diary can help with treatment and management. You can use a spreadsheet on your computer, notes on your phone, migraine tracking apps, or the good old notebook and pen, whichever works best for you.
Log the following details in your migraine journal:
Date and time of each migraine
Duration and intensity
What you ate in the 24 hours before the attack
Sleep patterns
Weather conditions
Stress levels
Medications taken and their effectiveness
I discovered what triggers my migraines and what measures have worked after several months of keeping a migraine journal. The details I wrote in my journal also helped my doctor prescribe the proper treatment for my migraines.
4. Practice Stress Management
Regular breaks: The 20-20-20 rule works wonders for me. That is, every 20 minutes, look at something 20 feet away for 20 seconds. It reduced my eye strain and the frequency of my headaches.
Movement: Take 5-minute breaks every hour when working. Do short walks or stretching to help prevent tension buildup from prolonged sitting and working in front of a computer. I set an hourly reminder to stretch my neck, arms, and wrists, plus a quick walk around my workspace just to keep the blood flowing.
Mindfulness practices: Even 5 minutes of deep breathing or meditation can reduce migraine frequency. I practice the 4-7-8 breathing for a few minutes when I feel stressed. This breathing technique is done by inhaling for 4 seconds, holding breath for 7 seconds, and exhaling for 8 seconds. I also practice yoga and meditation during my days off.
The Path to Migraine Relief Starts with Understanding Your Triggers
Understanding what triggers migraine puts you one step closer to gaining control over this challenging condition. As discussed above, triggers can range from environmental factors and lifestyle habits to specific foods and hormonal changes. Identifying migraine triggers and implementing ways to prevent them can significantly reduce the frequency and intensity of migraine attacks.
Remember that each person's migraine triggers are unique. What triggers my migraines (like the dreaded corn chips!) may not even bother you. Be patient and consistently track your migraine triggers and patterns through your migraine journal.
After knowing potential triggers, the next step is to learn how to manage the headaches and how to recover from migraine attacks. In my next post, I'll share coping strategies that helped me get through migraine attacks.
Until then, I encourage you to start identifying your triggers and implementing the preventive measures we've discussed. Stay tuned for my next post.
Which migraine trigger do you think affects you the most? Have you tried keeping a migraine journal yet? I'd love to hear about your experiences. Feel free to reach out through my contact page.
Disclaimer: This blog post is based on personal and professional experience and is intended for informational and educational purposes only. This is not a substitute for professional medical advice, diagnosis, or treatment. Always consult with your healthcare provider for specific questions or concerns regarding your health.
